Whole person wellbeing in a whole new way.
‘Best places to work’ companies have one thing in common – creating a culture of health that puts people first.
Nearly 90% of organizations agree they have a responsibility for the health and wellbeing of employees. That’s why high-performing companies around the world partner with us for an end-to-end solution that’s loved by businesses and employees alike.
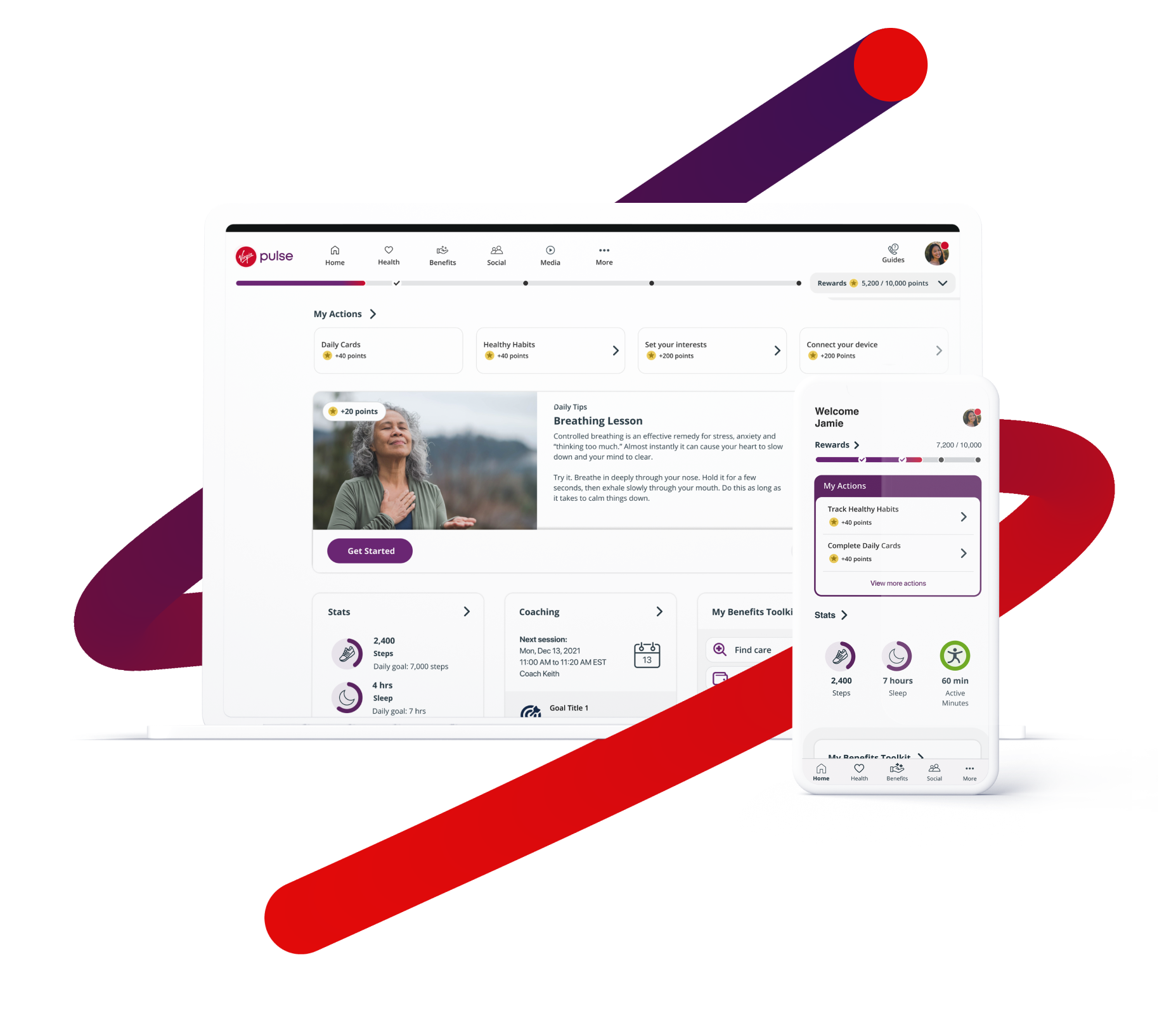
We provide a full-stack, mobile first platform that strengthens your culture, motivates your people and boosts your bottom line. We cover all dimensions of wellbeing as the single destination for easy access to benefits, live support, and incentives. Our data-driven, whole person support empowers individuals to make small, achievable changes that add up to big results and outcomes.
Give employees personal attention
Provide a self-serve digital experience that employees will use and love. They are always one-click away from vital human-interactions with live coaching, support, and more to become their best self.
Reduce the burden on your team
Our easy-to-use platform eliminates administrative work and multiple vendors, and significantly reduces benefit questions by empowering and supporting employees 24/7.
Improve benefit utilization and outcomes
Our data-driven personalization combined with gamification, daily nudges and behavior change science keeps employees engaged and ensures your investments pay off.
Foster a culture of belonging and collaboration
Cultivate community by celebrating differences and promoting inclusion and equity. Harness the power of social connection and increase collaboration with team-based initiatives and meaningful daily interactions.
-
65%
Of high risk members reduced their blood pressure
-
46%
Of members reported decreased stress levels
-
$1K
Reduction in health care claims cost per member per year
It’s time to activate change.
Request Demo → → → →